Health-care professionals
Clinical tips from the guideline
Symptoms
- Clinicians need to be aware of the clinical factors that increase the likelihood of endometriosis.
- The primary focus of investigation and treatment of endometriosis should be resolution of the presenting symptoms.
Diagnosis
- Pelvic pain that is not primary dysmenorrhea should be considered endometriosis until proven otherwise.
- Endometriosis should be considered early in the differential diagnosis of pelvic pain in young women since there is often a delay of 7 to 12 years from the onset of symptoms to definitive diagnosis.
- Investigation of suspected endometriosis should include history, physical and imaging assessments
- Routine CA-125 testing as part of the diagnostic investigation of endometriosis should not be performed.
- When suspecting deeply infiltrating endometriosis, a pelvic examination, including rectovaginal examination, is essential.
- The decision to move to surgery in women with pain and suspected endometriosis should be based on clinical evaluation, imaging, and effectiveness of medical treatment. The role of diagnostic laparoscopy should be limited.
- Imaging should be based on the clinical presentation and findings on physical examination.
Treatment
- In endometriosis treatment, all options should be administered for a minimum of 3 months, with evaluation of efficacy at the end of the trial.
- Combined hormonal contraception, ideally administered continuously, should be considered as a first-line therapy.
- Administration of progestin alone — orally, intramuscularly, or subcutaneously — may also be considered as first-line therapy.
- A GnRH agonist with add-back therapy, or an intrauterine system, should be considered as second-line therapy.
- Combined hormonal contraceptives are not appropriate for add back therapy.
- A GnRH agonist should be combined with HT add back therapy from commencement of therapy and may be considered for longer term use (> 6 months).
- While awaiting resolution of symptoms from the directed medical or surgical treatments for endometriosis, clinical judgment should be used in prescribing analgesics ranging from NSAIDs to opiates.
- With ovarian endometriomas it is important to consider the patient's desire for fertility. Removal of endometriomas requires an experienced operator since there is a risk of damaging the egg-containing ovarian cortex with subsequent diminished ovarian reserve.
- Ovarian endometriomas are often a marker of more extensive endometriosis.
Adolescents
- The approach to pelvic examination in adolescents should be flexible. Inspection, a rectoabdominal examination, and testing of the length of the vagina with a cotton-tipped swab can be used in non sexually active adolescents to investigate secondary dysmenorrhea.
Infertility
- Adherence to principles of microsurgery such as diligent hemostasis, reduced fulguration, and limited use of sutures may improve fertility.
- Excision is preferred over fenestration, drainage, or ablation of the cyst lining for the treatment of an ovarian endometrioma.
- Use of adhesion-prevention adjuncts may help reduce adhesion formation but improvement in fertility in unknown.
- Three months of suppression with a GnRH agonist and HT addback before IVF in women who have pelvic pain and infertility associated with endometriosis will greatly improve quality of life and reduce discomfort during ovarian stimulation and oocyte retrieval.
- Women with endometriosis-related infertility over the age of 35 years should be referred for IVF.
Evaluating pelvic pain
Tools for evaluating pelvic pain are available through the International Pelvic Pain Society (www.pelvicpain.org). For all patients with pelvic pain, a detailed pain and gynaecologic history should be taken to explore and rule out other causes of pain. Focused history-taking should also include reproductive health questions (age at menarch, cycle frequency and regularity, previous pregnancies, and use of oral contraception or hormonal treatments). Contributory medical and surgical history, as well as family history of endometriosis or gynaecologic cancers should be ascertained.
Management of pain associated with suspected endometriosis
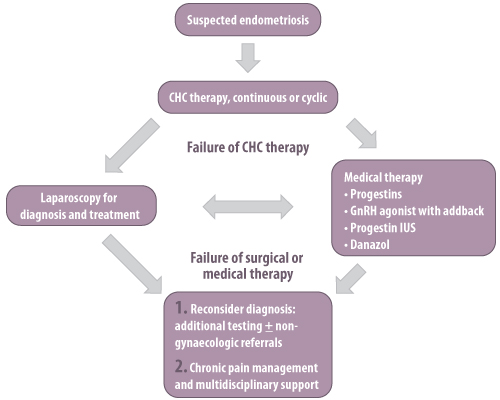
This flowchart is adapted from the SOGC's clinical practice guideline "Endometriosis".
Differential diagnosis for pelvic pain
Uterine
- Primary dysmenorrhea
- Adenomyosis
Bowel
- Irritable bowel syndrome
- Inflammatory bowel disease
- Chronic constipation
Bladder
- Interstitial cystitis
- Urinary tract infection
- Urinary tract calculi
Ovarian
- Mittelschmerz (ovulation pain)
- Ovarian cysts (rupture, torsion, etc.)
- Ovarian remnant syndrome
Fallopian tube
- Hematosalpinx (after sterilization or endometrial ablation)
- Ectopic pregnancy (acute or chronic)
- Pelvic inflammatory disease
General
- Endometriosis
- Myofascial pain
- Neuropathic pain
- Pelvic congestion
- Adhesions
This table is adapted from the SOGC's clinical practice guideline "Endometriosis".

